
A major component of Rein in Sarcoma’s mission is to fund research directed toward developing new treatments and finding cures for sarcoma cancers. Since our inception in 2001 RIS has funded nearly $2 million to sarcoma research projects, primarily at the University of Minnesota, with an expansion to the Mayo Clinic, Children’s Hospitals, and Clinics of Minnesota in 2017. These research dollars in turn have resulted in additional grants totaling over $13 million in public and private funding to date.
Research Grants
Click to learn about the research we have funded at top research institutions such as the University of Minnesota, Mayo Clinic, Children’s Hospitals, and Clinics of Minnesota.
Research News

2024-2025 Jan Maudlin Sarcoma Scholars
University of Minnesota William Shawn Morris completed his undergraduate degree in mechanical engineering from the

2023-2024 Jan Maudlin Sarcoma Scholars
University of Iowa Bri Iverson is a current M2 at the Carver College of Medicine.

Pediatric Sarcoma Research
We are proud to provide ongoing support to the University of Minnesota sarcoma researchers and investigators who have dedicated their careers to finding better treatments and ultimately a cure for sarcomas.

Seeking Leiomyosarcoma Patient Advocates
Seeking Leiomyosarcoma Patient Advocates to participate in the LMS Spore Research Project. The LMS SPORE
Register Now for the Sarcoma Research Symposium: Progress & Promise
We invite you to join us for the Minnesota Sarcoma Research Conference 2024, a hybrid
Save the Date: Annual Research Symposium
Save the Date: for the annual Rein in Sarcoma Research Symposium on March 28, 2024.
Sarcoma Doctors & Researchers
Meet the regional doctors and researchers involved in treating and researching sarcoma cancers. Click to read their profile.

u003ca href=u0022https://www.reininsarcoma.org/profile-dr-ed-cheng/u0022u003eDr. Ed Cheng, MDu003c/au003e
Department of Orthopedic SurgeryUniversity of Minnesota

u003ca href=u0022https://www.reininsarcoma.org/profile-chinsoo-cho/u0022u003eDr. Chinsoo Cho, MDu003c/au003e
Department of Radiation OncologyUniversity of Minnesota

u003ca href=u0022https://www.reininsarcoma.org/sarcoma-researcher-spotlight-dr-julie-chu/u0022u003eDr. Julie Chu, MDu003c/au003e
Hematology-Oncology physicianChildren’s Hospitals and Clinics of Minnesota

u003ca href=u0022https://www.reininsarcoma.org/profile-dr-denis-clohisy/u0022u003eDr. Denis Clohisy, MDu003c/au003e
Department of Orthopedic SurgeryUniversity of Minnesota

u003ca href=u0022https://www.reininsarcoma.org/profile-kathryn-dusenbery/u0022u003eDr. Katie Dusenbery, MDu003c/au003e
Department of Radiation OncologyUniversity Minnesota

u003ca href=u0022https://www.reininsarcoma.org/profile-dr-emily-greengard/u0022u003eDr. Emily Greengard, MDu003c/au003e
Department of PediatricsUniversity of Minnesota

u003ca href=u0022https://www.reininsarcoma.org/david-largaespada/u0022u003eDr. David Largaespada, PhDu003c/au003e
Department of PediatricsUniversity of Minnesota

u003ca href=u0022https://www.reininsarcoma.org/profile-nancy-mcallister/u0022u003eDr. Nancy McAllister, MDu003c/au003e
Pediatric OncologyChildren’s Hospitals and Clinics of Minnesota

u003ca href=u0022https://www.reininsarcoma.org/jaime-modiano/u0022u003eDr. Jaime Modiano V.M.D, PhDu003c/au003e
Department of Veterinary Clinical SciencesUniversity of Minnesota

u003ca href=u0022https://www.reininsarcoma.org/profile-dr-scott-okuno/u0022u003eDr. Scott Okuno MDu003c/au003e
Medical OncologistMayo Clinic

u003ca href=u0022https://www.reininsarcoma.org/christian-ogilvie/u0022u003eDr. Christian Ogilvie, MDu003c/au003e
Department of Orthopedic SurgeryUniversity of Minnesota

u003ca href=u0022https://www.reininsarcoma.org/profile-amy-skubitz/u0022u003eDr. Amy Skubitz, PhDu003c/au003e
Department of Laboratory Medicine and PathologyUniversity of Minnesota

u003ca href=u0022https://www.reininsarcoma.org/profile-dr-keith-skubitz/u0022u003eDr. Keith Skubitz, MDu003c/au003e
Hematology, Oncology and TransplantationUniversity of Minnesota

u003ca href=u0022https://www.reininsarcoma.org/profile-logan-spector-phd/u0022u003eLogan Spector, PhDu003c/au003e
Department of PediatricsUniversity of Minnesota

u003ca href=u0022https://www.reininsarcoma.org/profile-dr-subbaya-subramanian/u0022u003eDr. Subbaya Subramanian, MS PhDu003c/au003e
Department of SurgeryUniversity of Minnesota
u003ca href=u0022https://www.reininsarcoma.org/profile-brenda-weigelu0022u003eDr. Brenda Weigel, MD, MSCu003c/au003e
Department of PediatricsUniversity of Minnesota

u003ca href=u0022https://www.reininsarcoma.org/profile-felasfa-wodajo/u0022u003eDr. Felasfa Wodajo, MDu003c/au003e
Musculoskeletal Tumor SurgeryVirginia Cancer Specialists

u003ca href=u0022https://www.reininsarcoma.org/profile-randy-hurley/u0022u003eDr. Randy Hurleyu003c/au003e
u003cstrongu003eu003cemu003eOncology and Hematologyu003c/emu003eu003c/strongu003eRegions Hospital, HealthPartners
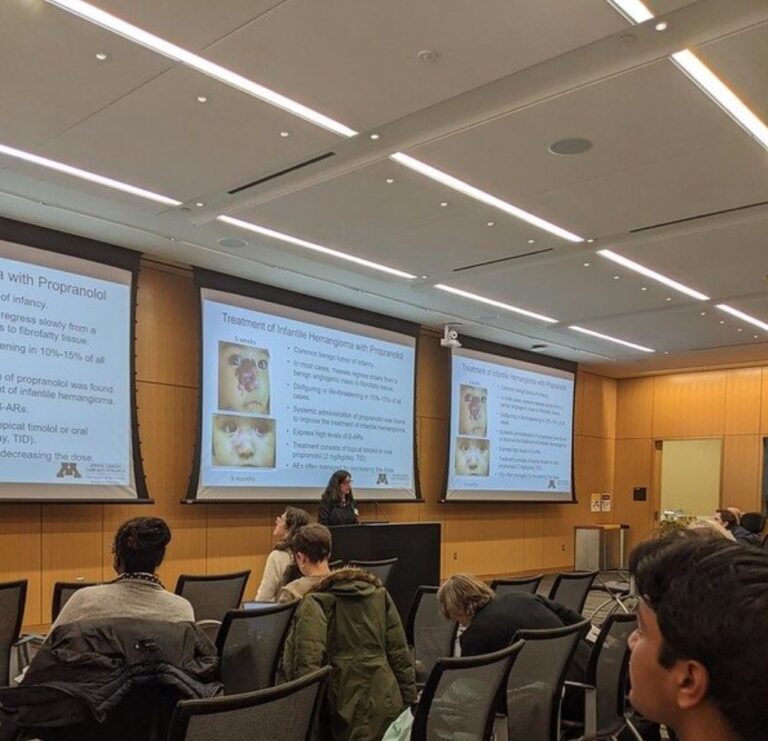
Progress and Promise: Minnesota Sarcoma Research Conference
The Progress and Promise Sarcoma Research Conference is a forum for researchers to share their findings to RIS stakeholders and students and further the collaboration among RIS-sponsored researchers. The event is sponsored by Rein in Sarcoma and the University of Minnesota Masonic Cancer Center.
